Why Is Exercise Important for Fibromyalgia?
Experts believe that exercise is essential for keeping muscles strong and flexible, controlling weight, and helping you stay active in other areas of life. In fact, exercise and activity allow patients to have some control over fibromyalgia and the amount of pain they feel.It used to be that doctors thought that exercise might worsen fibromyalgia symptoms or accelerate the disease. So doctors encouraged patients to seek rest, not activity. But recent scientific studies have shown that, for most patients, range of motion, strengthening, and aerobic conditioning exercises are safe and necessary.
Does Exercise Boost Endorphins in Those With Fibromyalgia?
Studies show that exercise helps restore the body's neurochemical balance and triggers a positive emotional state. Not only does regular exercise slow down the heart-racing adrenaline associated with stress, but it also boosts levels of natural endorphins -- pain-fighting molecules that may be responsible for the well-known "runner's high." Endorphins help to reduce anxiety, stress, and depression.Does Exercise Boost Serotonin in People With Fibromyalgia?
Serotonin is a neurotransmitter in the brain that scientists have found to be related to fibromyalgia. Neurotransmitters are brain chemicals that send specific messages from one brain cell to another. While only a small percentage of all serotonin -- 1% to 2% -- is located in the brain, this neurotransmitter is believed to play a vital role in mediating moods.Studies have found that too much stress can lead to permanently low levels of serotonin. That, in turn, can create aggression. An increased level of serotonin in the brain is associated with a calming, anxiety-reducing effect. In some cases it's also associated with drowsiness. A stable serotonin level in the brain is associated with a positive mood state or feeling good over a period of time. Lack of exercise and inactivity can aggravate low serotonin levels.
How Is Serotonin Related to Women and Fibromyalgia?
It appears that women may have a greater sensitivity to changes in this brain chemical. Mood swings during the menstrual cycle, menopause, or following the birth of a child may be hormonally induced through the action of the hormones on neurotransmitters.Various factors -- such as sunlight, certain carbohydrate foods, some hormones, and exercise -- can have a positive effect on serotonin. Exercise acts as nature's tranquilizer by helping to boost serotonin in the brain. Studies have also shown that exercise triggers the release of epinephrine and norepinephrine, hormones that are known to boost alertness. For those who feel "stressed out" frequently, exercise will help to desensitize your body to stress.
What Are Other Benefits of Exercise for Those With Fibromyalgia?
Regular exercise benefits people with fibromyalgia by doing the following:
- burning calories and making weight control easier
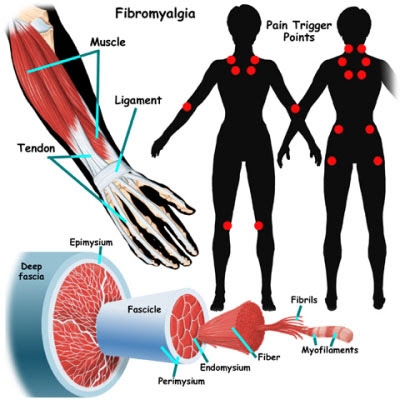
- giving range-of-motion to painful muscles and joints
- improving a person's outlook on life
- improving quality of sleep
- improving one's sense of well-being
- increasing aerobic capacity
- improving cardiovascular health
- increasing energy
- placing the responsibility of healing in the hands of the patient
- reducing anxiety levels and depression
- relieving stress associated with a chronic disease
- stimulating growth hormone secretion
- stimulating the secretion of endorphins or "happy hormones"
- strengthening bones
- strengthening muscles
- relieving pain
What Types of Exercises Work Best for Fibromyalgia Symptoms?
Some new findings suggest that exercises such as walking, strength training, and stretching activities are effective at improving physical, emotional, and social function. They also are effective in addressing key symptoms and self-efficacy in women with fibromyalgia who are also being treated with medication. Other studies point to long-term aquatic exercise programs -- such as water aerobics -- as being effective in reducing symptoms and improving the health-related quality of life of the participants.As you begin your exercise program, focus on three different types of exercise:
- Range-of-motion or stretching exercises:
- Endurance or conditioning exercises:
- Strengthening exercises:
Can Low-Impact Exercises Help Flexibility and Stress in Fibromyalgia?
Low-impact aerobic exercises have been shown to improve symptoms and restore muscle strength in people with fibromyalgia. Some helpful exercises include:- Yoga: an ancient form of exercise that can reduce stress and relieve muscular tension or pain by improving range of motion and strength. Practicing yoga for fibromyalgia when you are feeling tense or anxious may help you reduce stress and the risk of injury when you are on the job or at home.
- Tai chi: a series of flowing, graceful movements that can give you a good workout and stretching regimen. Studies show that tai chi participants also increase their sense of balance, can bend easier, and are better able to do household tasks. With fibromyalgia, tai chi can keep your back flexible and strong.
- Pilates: a form of exercise that focuses on breathing and strengthening the torso muscles. With Pilates, an instructor will help you work on postural muscles that are essential to supporting the spine.
Can Water Therapy Help People With Fibromyalgia?
Yes. If you have fibromyalgia, water therapy can give you good results. Water therapy strengthens and conditions as you move your body against the water. Water supports your weight during movement, which helps alleviate any impact on muscles and joints.The water alleviates the force of gravity and provides buoyancy as well as mild resistance. Whether stretching in the water, using a kickboard as a floatation device as you push and kick, or swimming using slow, gentle strokes, water therapy can provide a gentle form of conditioning. That makes it quite beneficial for people with fibromyalgia.
How Can I Get Started Exercising With Fibromyalgia?
If you have fibromyalgia and want to start exercising, it's important to start slowly. Begin with stretching exercises and gentle, low-impact activity, such as walking, swimming, or bicycling. Muscle soreness is normal when you are just starting an exercise regimen. But if you have sharp pain, stop and call your doctor. You may have overworked or injured your muscles.Are There Exercises to Avoid With Fibromyalgia?
There are no particular exercises to avoid if you have fibromyalgia. Aerobic exercise (running, jogging), weight training, water exercise, and flexibility exercises can all help. Golf, tennis, hiking, and other recreational activities are also healthful.If you have other medical problems or if you're planning more than a moderate-intensity exercise program, discuss your plan with your doctor before you start.